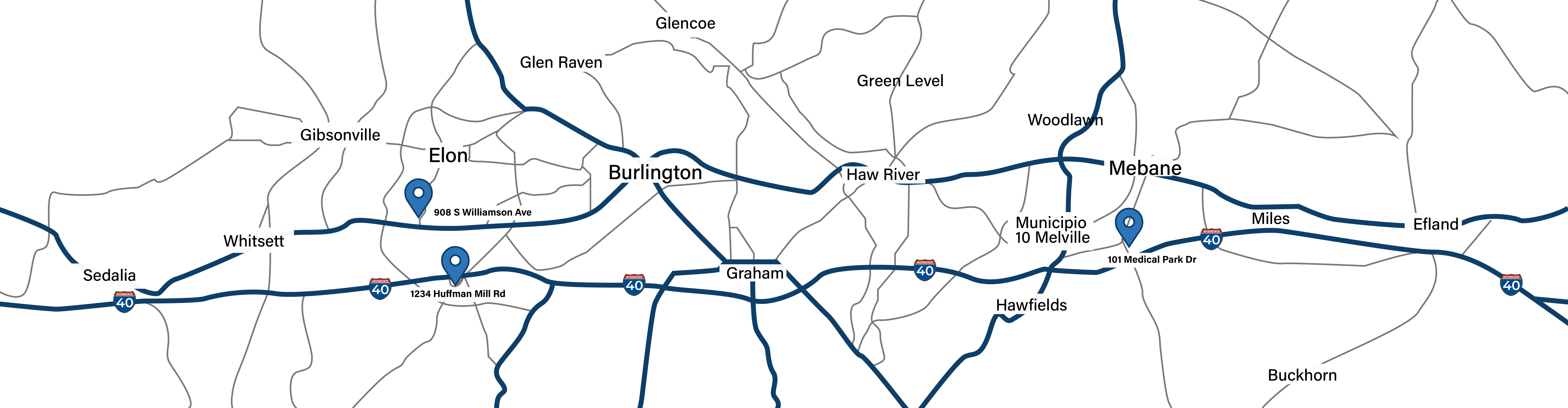
 Kernodle Clinic - A DukeMedicine PRACTICE
Kernodle Clinic - A DukeMedicine PRACTICE
- Burlington 336-538-1234
- Mebane 919-563-2500
- Elon Family 336-538-2314
- Elon Pediatrics 336-538-2416
How to Recognize the Symptoms of Ovulation: A Comprehensive Guide to Your Fertile Window
Ovulation is a key event in a woman’s menstrual cycle, marking the time when an egg is released from the ovary and is available for fertilization. Knowing when you ovulate is crucial for family planning, fertility awareness, and maintaining reproductive health. Many women, however, are unaware of the various physical symptoms that accompany ovulation. Recognizing these signs can help you better understand your body, whether you’re trying to conceive or avoid pregnancy. In this comprehensive guide, we’ll explore the common symptoms of ovulation, how to track them, and factors that may affect your ovulation cycle.
What Is Ovulation?
Ovulation occurs when a mature egg is released from one of the ovaries and travels through the fallopian tube, where it remains available for fertilization for approximately 12 to 24 hours. This process typically happens around the midpoint of your menstrual cycle, although the exact timing can vary depending on individual cycle length.
A typical menstrual cycle lasts between 21 and 35 days, and ovulation usually happens 12-16 days before the start of the next period. For example, in a textbook 28-day cycle, ovulation typically occurs around day 14. However, each woman’s cycle can vary, making it important to learn how to recognize the signs of ovulation specific to your body.
Why Is Tracking Ovulation Important?
Tracking ovulation can help you manage your reproductive health in several ways:
- Fertility awareness: If you are trying to conceive, knowing when you ovulate can help you time intercourse to increase the chances of fertilization.
- Natural contraception: If you prefer a natural method of birth control, tracking ovulation can help you avoid pregnancy by identifying your fertile window.
- Insight into menstrual health: Regular ovulation is a sign of a healthy menstrual cycle. Conversely, irregular or absent ovulation can be a sign of hormonal imbalances or underlying health issues.
By tracking ovulation, you can gain greater control over your reproductive health and address any concerns early on.
Common Symptoms of Ovulation
Women experience ovulation differently, but there are several common signs that can indicate you’re in your fertile window. Paying attention to these symptoms can help you better understand your cycle.
1. Changes in Cervical Mucus
One of the most noticeable signs of ovulation is a change in cervical mucus. As you approach ovulation, your body produces more cervical mucus to create a more favorable environment for sperm. During your fertile window, the mucus becomes clearer, stretchier, and slippery—resembling the consistency of raw egg whites. This type of mucus helps sperm travel more easily through the cervix and into the uterus.
Here’s a breakdown of how cervical mucus changes throughout your cycle:
- After your period: Cervical mucus is typically dry or absent.
- Approaching ovulation: Mucus becomes sticky, then creamy.
- During ovulation: Mucus becomes abundant, clear, and stretchy (egg-white consistency).
- After ovulation: Mucus becomes thicker or dries up again.
If you’re trying to track ovulation, monitoring changes in cervical mucus can be a simple yet effective way to identify your fertile window.
2. Mittelschmerz (Ovulation Pain)
Women who experience sharp or dull pain on one side of their lower abdomen during ovulation, a phenomenon known as Mittelschmerz (German for “middle pain”). This pain is caused by the rupture of the follicle when the egg is released from the ovary. Mittelschmerz can last anywhere from a few minutes to several hours and may switch sides each cycle, depending on which ovary releases the egg.
While Mittelschmerz is harmless, it can be uncomfortable. Some women also experience bloating or mild spotting during this time. If your ovulation pain is severe or persistent, it’s a good idea to consult with a healthcare provider, as it could be a sign of an underlying condition like endometriosis.
3. Basal Body Temperature (BBT) Increase
Tracking your basal body temperature (BBT)—your body’s lowest resting temperature—can provide a clear indication that ovulation has occurred. Before ovulation, your BBT is lower. After the egg is released, an increase in the hormone progesterone causes your BBT to rise by about 0.5 to 1.0 degrees Fahrenheit. This rise in temperature typically lasts until the start of your next period.
To track BBT:
- Use a basal thermometer, which is more sensitive than a regular thermometer.
- Take your temperature every morning at the same time, before getting out of bed or engaging in any activity.
- Track your temperature over several months to establish a pattern.
While BBT tracking can confirm that ovulation has occurred, it doesn’t predict when ovulation will happen. Combining BBT tracking with other methods, such as cervical mucus observation or ovulation predictor kits, can help you better identify your fertile window.
4. Heightened Sense of Smell
Some women report a heightened sense of smell around the time of ovulation. This increased sensitivity to certain scents, particularly male pheromones, may be due to hormonal changes that occur during the fertile window. While not a definitive sign of ovulation, a heightened sense of smell can be an additional clue for tracking your cycle.
5. Breast Tenderness
Breast tenderness or soreness is another common symptom of ovulation. Hormonal changes, particularly the increase in progesterone after ovulation, can cause the breast tissue to become swollen and sensitive. This tenderness may feel similar to the sensation some women experience before their period. If you notice regular breast tenderness around the same time each month, it could be linked to your ovulation cycle.
6. Light Spotting
Light spotting or discharge of brownish or pinkish blood around the time of ovulation can occur in some women. This is known as ovulation spotting, and it happens when the follicle ruptures and releases the egg. This symptom is generally harmless, but if you notice more frequent or heavier spotting between periods, it’s worth discussing with your healthcare provider to rule out other causes.
7. Increased Libido
Many women experience an increase in libido or sexual desire around the time of ovulation. This is thought to be nature’s way of encouraging reproduction. The surge in estrogen and luteinizing hormone (LH) leading up to ovulation may contribute to this temporary increase in sex drive. While not every woman experiences this symptom, an uptick in libido can be a good indicator that you’re in your fertile window.
8. Changes in Cervical Position
In addition to changes in cervical mucus, the position and texture of your cervix also change during ovulation. During your non-fertile days, the cervix is lower, firmer, and closed. As ovulation approaches, the cervix moves higher up, becomes softer, and opens slightly to allow sperm to pass through more easily.
Checking your cervical position takes practice and consistency. Here’s how to check:
- Wash your hands thoroughly.
- Insert a clean finger into your vagina and feel for the cervix.
- Track how the position and texture of your cervix change throughout your cycle.
Over time, you’ll be able to identify patterns that can help predict ovulation.
Less Common Symptoms of Ovulation
While the symptoms listed above are the most common signs of ovulation, some women may experience other, less common symptoms. These may include:
- Headaches or migraines: Hormonal fluctuations during ovulation can trigger headaches or migraines in some women.
- Bloating: Ovulation-related bloating is often caused by hormonal changes, particularly the rise in estrogen and LH, which can lead to water retention.
- Nausea: Some women report feeling nauseous around the time of ovulation, possibly due to the hormonal shifts that occur during this phase of the menstrual cycle.
If you experience any of these less common symptoms and find them disruptive to your daily life, it’s a good idea to discuss them with your healthcare provider.
Hormonal Changes During Ovulation
Ovulation is triggered by a complex interaction of hormones. Understanding these hormonal changes can help you better recognize the signs of ovulation.
1. Follicle-Stimulating Hormone (FSH)
At the start of your menstrual cycle, the pituitary gland releases follicle-stimulating hormone (FSH), which stimulates the growth of ovarian follicles. Each follicle contains an immature egg, but only one follicle will mature and release an egg during ovulation.
2. Luteinizing Hormone (LH)
As the dominant follicle matures, it produces increasing amounts of estrogen. The rise in estrogen levels triggers a surge in luteinizing hormone (LH), which causes the mature follicle to rupture and release the egg. The LH surge typically occurs about 24-36 hours before ovulation, making it a key indicator of your fertile window.
3. Estrogen and Progesterone
Before ovulation, estrogen levels are high, which contributes to symptoms like increased cervical mucus and changes in libido. After ovulation, progesterone levels rise to prepare the body for a potential pregnancy by thickening the uterine lining. Progesterone is responsible for the post-ovulation rise in basal body temperature and can also cause symptoms like breast tenderness.
Tools for Tracking Ovulation
If you want more precise information about when you’re ovulating, there are several tools you can use to supplement your symptom tracking.
1. Ovulation Predictor Kits (OPKs)
Ovulation predictor kits (OPKs) measure the levels of luteinizing hormone (LH) in your urine. Since the LH surge occurs right before ovulation, a positive result indicates that ovulation is likely to occur within the next 12-36 hours. OPKs are highly accurate and are a useful tool for predicting ovulation, especially if you have irregular cycles.
2. Fertility Apps
Fertility tracking apps can help you record your symptoms, basal body temperature, and other ovulation signs to predict your fertile window. Many apps use algorithms to provide personalized predictions based on your cycle data. Popular fertility apps include Clue, Ovia, and Glow.
3. Ultrasound and Blood Tests
In some cases, your healthcare provider may recommend an ultrasound or blood test to monitor ovulation. Ultrasound can confirm the presence of a mature follicle, while blood tests can measure hormone levels to determine if ovulation is occurring.
Factors That Can Affect Ovulation
Several factors can influence the timing and regularity of ovulation. Some women experience irregular cycles or difficulty ovulating due to underlying health conditions or lifestyle factors.
1. Polycystic Ovary Syndrome (PCOS)
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that can disrupt ovulation. Women with PCOS often have irregular or absent periods, as their ovaries may not release eggs regularly. Other symptoms of PCOS include acne, weight gain, and excess facial or body hair.
2. Thyroid Disorders
Both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) can affect ovulation. Thyroid hormones play a key role in regulating the menstrual cycle, and imbalances can lead to irregular ovulation or amenorrhea (absence of periods).
3. Stress and Lifestyle Factors
Stress, excessive exercise, and significant weight changes can all impact ovulation. High levels of stress can interfere with the release of reproductive hormones, while extreme exercise or rapid weight loss can suppress ovulation altogether.
4. Age
As women age, the number of eggs in their ovaries declines, and ovulation becomes less regular. By the time a woman reaches her late 30s or early 40s, she may notice that her cycles become shorter, longer, or more irregular.
When to See a Healthcare Provider
If you’re having trouble identifying ovulation symptoms, or if you suspect you’re not ovulating regularly, it’s important to see a healthcare provider. Conditions like PCOS, thyroid disorders, or other hormonal imbalances may require treatment to restore regular ovulation.
If you’re trying to conceive and haven’t been successful after a year of unprotected intercourse (or six months if you’re over 35), it’s a good idea to speak with a fertility specialist.
Conclusion
Understanding the symptoms of ovulation can help you take control of your reproductive health, whether you’re trying to conceive, avoid pregnancy, or simply gain a better understanding of your menstrual cycle. By paying attention to changes in cervical mucus, basal body temperature, and other physical signs, you can accurately predict your most fertile days and plan accordingly.
If you’re struggling to detect ovulation or have concerns about irregular cycles, consulting with a healthcare provider can help address any underlying issues. Tools like ovulation predictor kits, fertility apps, and medical evaluations can also provide valuable insights into your ovulation patterns. Tracking ovulation consistently over time allows you to make more informed decisions about your health and family planning.